Article
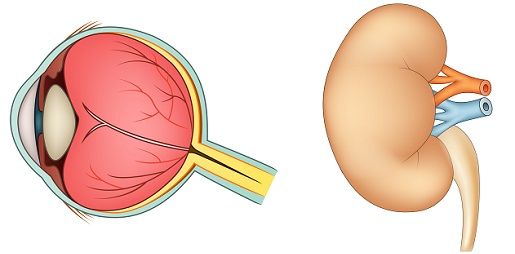
Tubulointerstitial Nephritis and Uveitis Syndrome Threatens Vision in Some Patients
Author(s):
Some cases of tubulointerstitial nephritis and uveitis syndrome, or TINU, have a poor visual prognosis, so early diagnosis and treatment are recommended. Diagnosis requires detailed history taking, whole-body imaging studies, and examination of renal function.
A team from the Department of Ophthalmology and Visual Science at the Yokohama City University Graduate School of Medicine in Yokohama, Japan, recently published an online case report series that detailed three different clinical manifestations of tubulointerstitial nephritis and uveitis syndrome, or TINU.
Although rare, TINU occurs in both Asians and Caucasians. Since TINU was first reported in association with myeloid sarcoma in 1975, hundreds of cases unassociated with myeloid sarcoma have been reported.
Diagnostic criteria for TINU include uveitis and acute tubulointerstitial nephritis, itself a kidney disorder, confirmed histopathologically in the absence of systemic diseases like sarcoidosis, which are often associated with TIN, uveitis, or both. Patients with TINU usually have bilateral uveitis with an acute onset. Uveitis often becomes chronic or recurrent, and patients may have a slight fever, the most common systemic symptom of TINU.
TINU is most likely to affect girls who have not yet reached puberty. It affects females more than males (sex ratio, 2.5:1) and accounts for 1% to 2% of uveitis cases in children ≤15 years of age. However, it sometimes affects the middle-aged, in whom it tends to be chronic.
The first case in the series was that of a 15-year-old boy with left eye pain and iridocyclitis, reduced visual acuity, and flu-like symptoms. Hospital staff noted 1+ inflammatory cells in the anterior chamber, so they classified the disease as bilateral anterior uveitis. In addition, both eyes had fine keratic precipitates. These indicate that the uveitis is non-granulomatous, which differentiates early TINU from sarcoidosis-related uveitis, which is granulomatous.
Blood tests and urinalysis revealed elevated creatinine and markedly increased levels of β2-microglobulin (β2MG) and N-acetyl-β-D-glucosaminidase (NAG), a marker of renal dysfunction in TINU. Together, elevated creatinine and β2MG have a positive predictive value of 100% for detecting TINU.
In addition, abdominal plain computed tomograms showed mild enlargement of both kidneys, and renal biopsy results indicated diffuse infiltration of inflammatory cells from the tubulointerstitium to the medulla. Such infiltration is a typical feature of TIN, and these and the laboratory findings led to a diagnosis of TINU.
The patient received methylprednisolone, 1,000 mg/day for three days, and oral prednisolone, 30 mg daily, which was tapered. By Day 40, anterior uveitis had improved, but when the dosage was reduced to 10 mg daily, uveitis recurred, and β2MG and NAG levels increased, so staff decided to continue ocular and oral steroids.
The second case was that of a 14-year-old girl with right eye pain and bilateral iridocyclitis. Upon referral to the hospital, staff found no inflammation in the anterior chamber but fine keratic precipitates in both eyes. They also detected bilateral edema of the optic disks. They classified the disease as anterior uveitis with bilateral papilledema.
Fluorescein angiography (FA) showed leakage from the optic disks and retinal veins of both eyes, which is a common finding in TINU. Moreover, because computed tomography did not show swelling of the optic nerve, the diagnosis of optic neuritis was excluded.
Although results of initial urinalysis were normal, repeated urinalysis three months later showed elevated levels of β2MG and NAG. These additional findings led to a diagnosis of TINU.
Right papilledema improved after the patient received an injection of triamcinolone acetonide in the sub-Tenon’s capsule. Despite continued treatment with an ocular steroid, left papilledema worsened but later resolved along with renal dysfunction despite a lack of systemic treatment.
The third case is that of a 49-year-old woman with right eye pain and iridocyclitis. After she was referred to the hospital, staff found 2+ inflammatory cells in the right anterior chamber, moderate to small keratic precipitates, and peripheral anterior synechiae, typical in recurring or prolonged TINU, in both eyes. The disease was classified as panuveitis.
Staff also noted optic disk edema and macular edema in the right eye. FA showed a hyperfluorescent right optic disk, cystoid macular edema, and leakage from the peripheral retinal veins, as in Case 2.
The patient had been diagnosed with TIN a year earlier and had received oral prednisolone. Based on this diagnosis and the presence of uveitis, the staff diagnosed the disease as TINU. Ocular steroid therapy relieved anterior ocular disease and macular edema that occurred first in the right eye and then in the left.
In a final comment, the team noted that, although TINU generally has a favorable prognosis, choroidal neovascularization sometimes develops, so they recommend early diagnosis and treatment.
The team published this case report series, “Three cases of tubulointerstitial nephritis and uveitis syndrome with different clinical manifestations,” online in International Ophthalmology on August 10, 2016.
Related Coverage:
Women with Spondyloarthritis Face Increased Risk of Uveitis, Other Conditions
Prognosis Fairly Good for Kids with Juvenile Idiopathic Arthritis





