Publication
Article
Family Practice Recertification
What is Causing This Woman's Abdominal Discomfort?
Author(s):
This is 52-year-old woman presented to the emergency with department with a 4-day history of upper abdominal cramping pain, nausea, vomiting, and distended abdomen.
James D. Collins, MD
History
This is a 52-year-old woman presented to the emergency department with a 4-day history of upper abdominal cramping pain, nausea, vomiting, and distended abdomen. Her past medical history was notable for having undergone a total abdominal hysterectomy and bilateral salpingo-oophorectomy for adenocarcinoma of the endometrium 2 months earlier. Abdominal plain radiographs were obtained.
Radiographic Findings
The upright anterior posterior (AP) abdominal radiograph (FIGURE 1) displayed hazy bilateral pleural effusions, coiled-spring appearance of the valvulae conniventes in the dilated stepladder air fluid levels in the edematous small bowel, faint display of calcified mesenteric lymph nodes, air in a hiatal hernia, and obscuration of the psoas margins consistent with ascites. The supine abdominal radiograph (FIGURE 2) displayed the degenerative changes of the lumbosacral spine, edematous mucosa of the stomach, low position of the large bowel in the pelvis post total hysterectomy and bilateral salpingo-oophorectomy for adenocarcinoma of the endometrium. FIGURE 3, inverted image, provided a different perspective revealing a hiatal hernia, haustral landmark anatomy of the large bowel low in the pelvis post-surgery as above and confirmation of bilateral pleural effusions.
Diagnosis: Mechanical small bowel obstruction, ascites, and bilateral pleural effusions.
Discussion
The causes of bowel obstruction may be mechanical or non-mechanical. The former are subdivided into lesions extrinsic to the intestine (such as adhesions and external hernias), intrinsic to the intestinal wall (such as diverticulitis and carcinoma), and those that
obstruct the lumen (as with a gallstone). The most common causes of small bowel obstruction are adhesions as a result of previous abdominal surgery and external hernias as in our patient. The latter two above causations two account for almost three quarters of small bowel obstructions. In contrast are the most frequent causes of colonic obstruction— carcinoma, sigmoid diverticulitis, and volvulus in that order.1
Adynamic ileus is the most important non-mechanical or hormonal cause of abdominal obstruction. Its development is mediated through the hormonal component of the sympathoadrenal system.1 The differential should also include jejunal diverticulosis, which may appear as multiple air-fluid levels, but the patient is usually asymptomatic.
Characteristics of small bowel obstruction include dilated (greater than 3 cm) loops of many valvulae conniventes in the jejunum, an ileum that appears smooth with no transverse indentations,2 and many air fluid levels that may have a stepladder appearance
on an upright film (Figure 1). The more proximal the obstruction, the more severe the pain and the more intense the vomiting. At the same time, small bowel obstruction produces a lesser degree of abdominal distension. Hiccups are also a common symptom. If small bowel obstruction is complete, there will be few air fluid levels in the colon; if it is partial, air fluid levels may be present. A coiled-spring pattern in the distended bowel may also be evident (Figure 2).
Characteristics of colonic obstruction include less intense pain and vomiting than with small bowel obstruction, 1 marked abdominal distension, lumen diameter greater than 5 cm on plain upright and supine films, haustra incompletely crossing the bowel wall,
colonic gas, and few fluid levels. Descending colonic obstruction may occasionally present a confusing picture if the ileocecal valve is incompetent. Radiographs with the patient in upright, supine, and decubitus positions facilitate identification of the obstructed segment.1-3
Take-home Message
In adults, plain radiographs can reliably identify small bowel obstruction by site, specific radiographic signs, and architectural abnormalities. Characteristics to look for include fluid and bowel gas in dilated loops of the small bowel, often in a step ladder arrangement. A coiled spring appearance is also likely.

Figure 1 This upright abdominal view displays air-fluid (AF) levels in the
lumen of the small bowel, hiatal hernia (H), and the irregular right pleural effusion in the posterior sulcus (not labeled). Observe the faint calcified mesenteric lymph node (arrows) and its changed position compared with Figure 2 ). E= left pleural effusion; I = Ilium; LV = left ventricle; P = pulmonary artery; R =right; T12 = 12th thoracic vertebra.
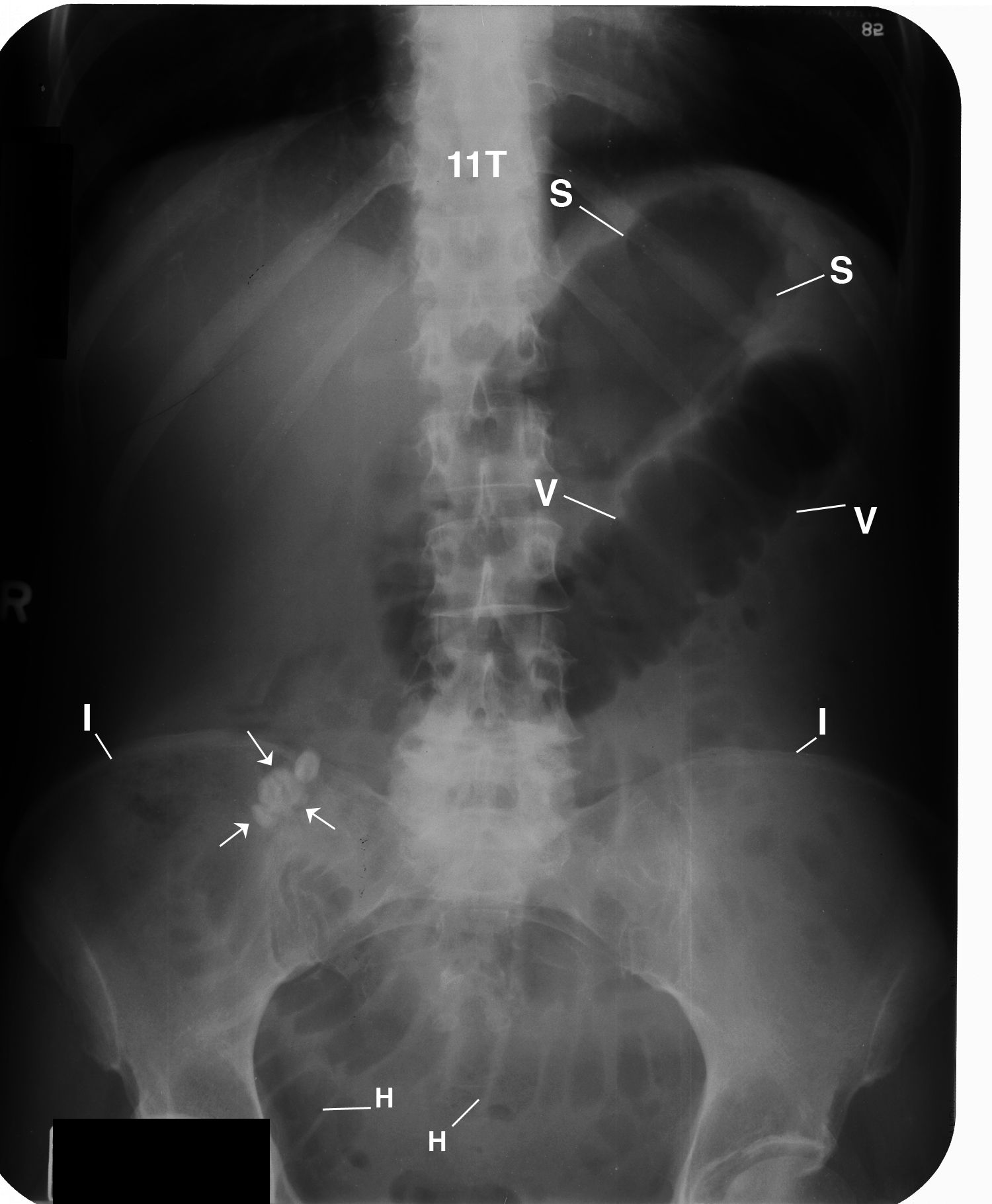
Figure 2 This anterior posterior (AP) supine abdominal radiograph displays hazy fluid
in the dilated stomach (S) and a coiled-spring appearance of the valvulae
conniventes (V) in the dilated loops of the small bowel. Observe the faint
density of the sharply marginated calcified lymph node (arrows) within
the mesentery over the right ilium (I). H= Haustra of the large intestine; LD = left hemidiaphragm; LV = left
ventricle (LV), L5 = fifth lumbar vertebrae; RD = right hemidiaphragm;
T11 = 11th thoracic vertebra.
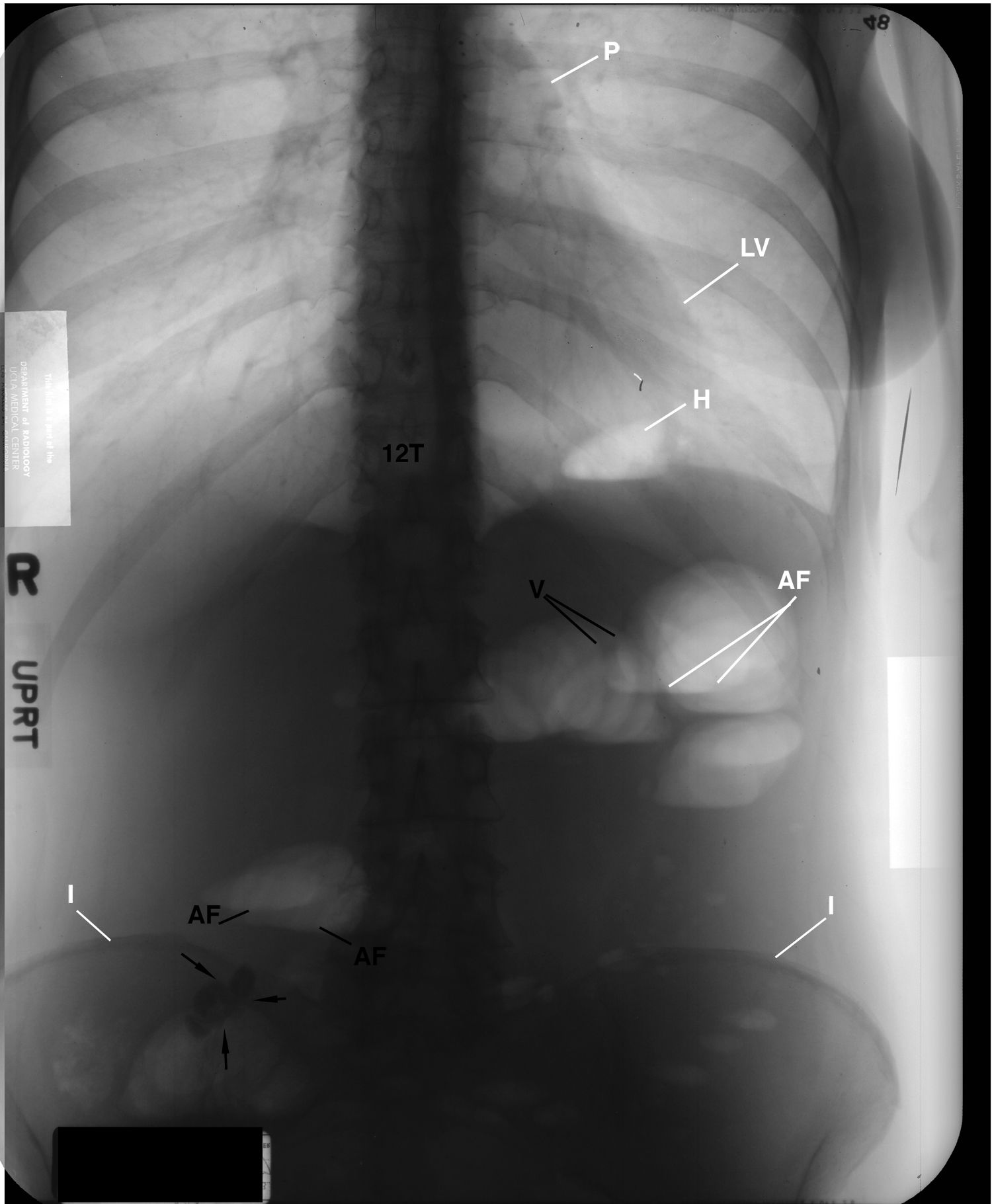
Figure 3. This is the inverted image of Figure 1 that provides a different perspective displaying a hiatal hernia (H) and straightening of the left pericardium between the margins of the pulmonary artery (P) and the left ventricle (LV) reflecting fibrosis (not labeled).
References
1. Silen W. Acute intestinal obstruction. In: Kasper DL,
Braunwald E, Fauci AS, et al. Harrison’s Principles of Internal
Medicine. 16th ed. New York, NY: McGraw-Hill; 2005:
1803-1805.
2. Meschan I. Analysis of Roentgen Signs in General Radiology.
Philadelphia, Pa: WB Saunders Co; 1976:552-590.
3. Robbins LL, ed. Golden’s Diagnostic Roentgenology. Vol 2.
Baltimore, Md: Williams & Wilkins; 1961:265-343C.
About the Author
James D. Collins, MD, is Professor and General Radiologist in the Department of Radiology at the UCLA David Geffen School Medicine. He formerly served as Director of the required medical student training for the department and President of the James T. Case Radiologic Foundation.
Collins has an extensive background of publications, consultations, and editorial positions, including his current post as the Radiology Editor for the Journal of the National Medical Association. He specializes in bilateral 3-dimensional MRI, MRA, and MRV imaging of the brachial plexus and has been performing those studies since 1985.