Publication
Article
Family Practice Recertification
A 35-Year-Old Man Presents with Non-cardiac Chest Pain and Severe Hypertension
Author(s):
A 35 year-old man with a history of hypertension, obstructive sleep apnea and obesity presents to clinic with complaints of non-cardiac chest discomfort. He is requesting refills of his blood pressure medications. His insurance changed 6 months ago and he has not had them since. The nurse performs the intake vital signs and reports that the patient has a blood pressure of 280/150 mmHg.
A 35 year-old man with a history of hypertension, obstructive sleep apnea and obesity presents to clinic with complaints of non-cardiac chest discomfort. He is requesting refills of his blood pressure medications. His insurance changed 6 months ago and he has not had them since. The nurse performs the intake vital signs and reports that the patient has a blood pressure of 280/150 mmHg.
The patient is no distress. A repeat blood pressure after resting in a chair for 5 minutes with feet resting on the floor and his arm at heart level reveals a pressure of 254/121. Exam is notable for bounding pulses and a laterally displaced point of maximal impulse during chest palpation. An EKG is performed in the office and is shown below (Figure). He is subsequently sent to the emergency department where serial EKGs are identical in morphology.
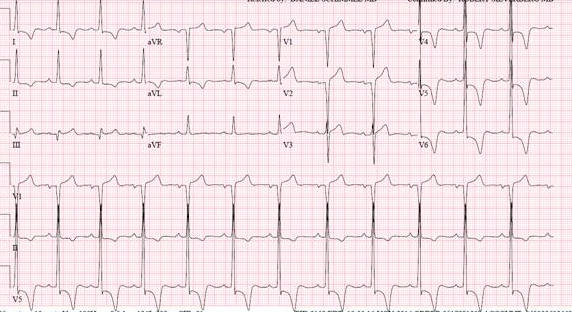
The EKG demonstrates a normal sinus rhythm with a rate of 72 bpm. It is immediately notable for large amplitude waveforms, distinctly abnormal T waves that are inverted in the lateral leads with down-sloping ST segment depression and ST segment elevation in the precordial leads V2-V3.
The findings are most consistent with left ventricular hypertrophy (LVH) and associated repolarization abnormalities.
Criteria for LVH: voltage-based criteria sufficient for diagnosis (without repolarization abnormalities)
1. Cornell Criteria (most accurate): Sum of R in aVL and the S wave in V3 greater than 20 in a woman or 28 in a man
2. Modified Cornell Criteria: R in aVL greater than 12 mm
3. Sokolow-Lyon Criteria: Sum of S wave in V1 and R wave in V5 or V6
a. > 35 mm if age > 40 years
b. > 40 mm if age 30-40 years
c. > 60 mm if 16-30 years
4. Other criteria relying on single leads exist, but the above are the most commonly used and most accurate.
Applying the above criteria to the EKG in question, the patient has LVH by the Sokolow-Lyon Criteria.
LVH can also significantly affect the repolarization patterns on an EKG. Physicians frequently attribute ST segment and T wave abnormalities to ischemia or infarction rather than the changes associated with LVH. In the setting of severe hypertension and questionable chest pain, its diagnostic utility for immediate risk stratification becomes compromised. The repolarization abnormalities associated with LVH are listed below and seen in the presented patient.
Associated repolarization abnormalities:
1. QRS abnormalities (in addition to LVH criteria above)
a. qS pattern in V1-V2
b. Tall R waves in lateral leads
c. Widening of the QRS
d. Depression of the J point
2. T wave abnormalities
a. T wave inversion in the lateral leads (leads I, aVL, V5-V6)
b. Biphasic T waves (initial part negative with terminal portion positive) may also be seen in the lateral leads
3. ST segment deviation
a. Horizontal or down-sloping in the lateral leads (“strain” pattern)
b. Elevation in precordial leads V1-V3
Although there are a number of ways to evaluate for LVH listed above, one algorithm utilizes both voltage criteria and the repolarization pattern to improve the specificity for diagnosis.
Romhilt-Estes Criteria: If sum of below findings is 4, then LVH is possible with 50% sensitivity. If sum of below findings is 5 or greater, LVH is likely with specificity of approximately 90%.
a. Amplitude of largest R or S in limb leads ≥ 20 mm = 3 points
b. Amplitude of S in V1 or V2 ≥ 30 mm = 3 points
c. Amplitude of R in V5 or V6 ≥ 30 mm = 3 points
d. ST and T wave changes opposite QRS without digoxin = 3 points
e. ST and T wave changes opposite QRS with digoxin = 1 point
f. Left atrial enlargement = 3 points
g. Left axis deviation = 2 points
h. QRS duration > 90 ms = 1 point
i. Initial deflection in V5 or V6 > 50 ms = 1 point
Although it can be tempting to invoke diffuse myocardial ischemia in a pattern like the presented EKG, the clinical story is not consistent with a severe ischemic presentation. If the history is suggestive for ischemia, severe hypertension can cause diffuse subendocardial ischemia and may be associated with ST elevations in aVR and may have dynamic changes in the ECG associated with fluctuations in blood pressure. The presented patient has no cardiac symptoms and no aVR elevations. Given his lack of symptoms, he has accelerated hypertension without acute end-organ damage, or hypertensive urgency and the ECG is most consistent with LVH and strain pattern.
The sensitivity to diagnose LVH by voltage criteria can be impaired by obesity, COPD, pneumothorax, pericardial or pleural fluid or fibrous tissue as seen in sarcoid or amyloid disease. Specificity diagnosis of LVH by amplitude criteria is reduced in patients with a thin habitus, a history of mastectomy, LBBB, or Wolf-Parkinson White pattern. Over-diagnosis of LVH can also occur in younger patients if age is not taken into consideration in the voltage criteria (as described above).
Because of the severe elevation in blood pressure, the patient was admitted for titration of medication with a goal to gradually reduce his blood pressure. In the emergency department, he was given a sublingual nitroglycerin and nitropaste followed by a nicardipine drip. On admission, his oral regimen was captopril given every 6 hours, followed by his home doses of amlodipine and thiazide. The captopril was transitioned to lisinopril and he was discharged by hospital day 3 with a systolic blood pressure averaging 150-160 mmHg. Further titration was planned as an outpatient. An outpatient secondary work-up for hypertension was negative.
1. Birnbaum Y, Alam M. LVH and the diagnosis of STEMI — How Should We Apply the Current Guidelines? Journal of Electrocardiography. 2014; 47(5):655-660
2. Brady WJ, Chan TC, Pollack M. Electrocardiographic Manifestations: Patterns that Confound the Diagnosis of Acute Myocardial Infarction — Left Bundle Branch Block, Ventricular Paced Rhythm, and Left Ventricular Hypertrophy. Journal of Emergency Medicine. 2000; 18(1):71-78 .
3. O’Keefe JH, Hammill SC, Freed MS, Pogwidz SM. The Complete Guide to ECGs: A Comprehensive Study Guide to Improve ECG Interpretation Skills. Sudbury: Jones and Bartlett Publishers, 2008. Print.
About the AuthorDaniel R. Schimmel, MD MS is an interventional cardiologist at Northwestern Memorial Hospital and assistant professor at the Northwestern University Feinberg School of Medicine. His clinical interests include acute cardiac care, coronary and peripheral interventions, structural heart disease, venothromboembolic disease and cardiovascular imaging. Having been a chief resident and chief fellow at Northwestern University he is dedicated to education with a research focus in simulation-based medical education. During his training years, Dr. Schimmel was recognized several times with the Excellence in Teaching Award. He also obtained his Master’s of Science in Clinical Investigation from Northwestern University and a certificate in quality and safety improvement.