Publication
Article
Cardiology Review® Online
Malpractice Risk According to Physician Specialty
Gregory S. Pokrywka, MD, FA CP, FN LA, NCMP
REVIEW
Jena et al, “Malpractice risk according to physician specialty,” N Engl J Med. doi:10.1056/ NEJMsa1012370. February 2012 | Cardiology Review 33 FEATURE | Malpractice Risk review Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365:629-636.
M
alpractice risk is a daily concern for all physicians, yet surprisingly little is known about the differences between medical specialties with respect to the annual incidence of claims, size of payments, and cumulative career incidence of claims. The few studies that exist are limited by their use of older data, limited geographic coverage, reliance on self-reports, small sample sizes, low response rates to surveys, limited physician specialty information, and lack of payment size data. Although the National Practitioner Data Bank includes most US cases in which a plaintiff was payed on behalf of a licensed health care provider, it does not report physician specialty and does not record data on cases that do not result in a payment.
Study Details
The authors were funded by the RAND Institute of Civil Justice and the National Institute on Aging. They examined physician-level data from a large physician- owned professional liability insurer covering physicians in all 50 states and the District of Columbia. The data are relatively current and large, covering closed malpractice claims for 40,916 physicians from 1991 to 2005 (233,738 physician-years of coverage). Physicians between the ages of 30 and 70 years were included in the study; the average age of physicians in all specialties was 49.0 years (range, 43.2 for emergency medicine to 53.0 for gynecology). Data on sex and race were not available.
Twenty-four specialties with at least 200 physicians each were identified; physicians in other, smaller specialties were grouped together in an “other specialty” category. California was overrepresented in this data (39.3% of the physicians), but after a reweighting process this share dropped to only 12.2%. Mean and median payments reflected indemnity payments made at jury verdicts or settlement with the claimant, and an outlier group of payments in excess of $1 million was identified. Data were separated into 3 time periods, 1991-1995, 1996-2000, and 2001-2003. “High-risk” and “low-risk” specialties were defined as the 5 specialties with the highest and lowest proportions of physicians with a claim in each category. Physician age data was used to calculate an annual rate of facing a claim, and was categorized by physician age and specialty. This model assumed that the probability of being sued was unrelated to the duration of coverage by this insurer, and that the probability of being sued at a given age was independent of being sued at an earlier age.
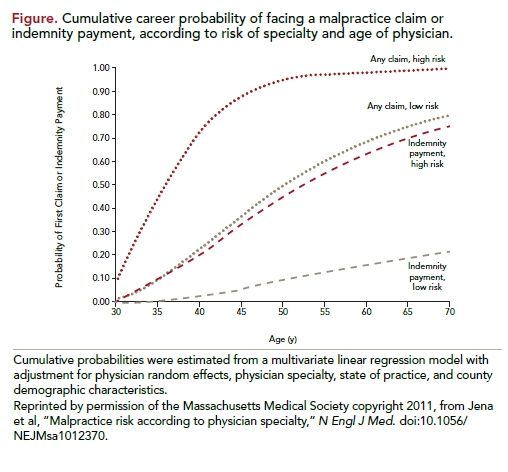
A total of 7.4% of all physicians annually had a malpractice claim, with significant variability across specialties: from 2.6% in psychiatry to 19.1% in neurosurgery. Annually, 1.6% of physicians made an indemnity payment, but the specialties in which physicians were most likely to face claims were not always the specialties in which indemnity claims occurred most often. The proportion of physicians with a claim was not well correlated with the payment rate, which was the number of physicians with a payment divided by the number with a claim (Pearson’s correlation, 0.17; P = 0.42). As an example, gynecology had the 12th highest claim rate, yet had the highest payment rate of >38%. With respect to time periods, differences in overall and paid claims were stable between low-risk and high-risk specialties. However, the annual claim rate in low-risk specialties actually decreased between 1991 and 1995 and 2001 and 2003. Average payment did not correlate well with claim rate (Pearson’s correlation, 0.13; P = 0.52), a finding the authors say suggests that the factors influencing the likelihood of a claim are independent of the factors that drive the size of the payment. Outlier awards (>$1 million) were infrequent, accounting for less than 1% of all payments, with obstetrics and gynecology accounting for the most payments. By age 65, a high percentage of physicians will face a claim (75% of those in low-risk specialties and 99% of those in high-risk specialties); the risk of indemnity payments at age 65 is 19% and 71%, respectively (Figure). Significant heterogeneity existed among specialty-specific projections of career malpractice risk.
COMMENTARY
Malpractice Risk and Specialty
T
his analysis of a large malpractice claims database demonstrates substantial heterogeneity across physician specialties in all risk parameters examined. Almost all high-risk specialty physicians will have a claim during their careers, but a substantial minority will not have to make a claims payment. A surprising finding is that specialties in which the largest proportion of physicians faced a claim were not necessarily those with the highest average payment size. Also important is the finding that a high percentage of claims do not result in payments to the plaintiff. Given that physician concern varies much less considerably across states than the objective measures of malpractice risk according to state, what accounts for this disparity?
Cardiologists and internists are in the middle of the pack in terms of the proportion of physicians facing claims annually, both coming in slightly higher than the average for all physicians. The rate of claims with indemnity payments is slightly less for cardiologists than for internists and all physicians, perhaps a surprising result in light of the increased amount of life-threatening and acute care rendered by cardiologists relative to the other specialties. This further illustrates the study’s conclusion that the forces that apparently drive claims differ from those that drive payments. Median physician indemnity payments to plaintiffs are higher for internists than for cardiologists, again illustrating this point.
Despite the soundness of study design and interesting analysis of this data, its insights are of little use in the busy clinician’s practice, other than as a vindication for the perceived high risk of medical malpractice we all face daily. As the authors point out, physicians can protect themselves from indemnity payments with malpractice insurance, but there is no protection from the time lost, stress, lost income, additional labor, and damage to reputation that result from a claim. Being the best doctors we can be, technically and in our interactions with patients and family, is our charge every day. It cannot be overemphasized how important it is to listen to our patients and respect them—2 of the best ways we can all prevent malpractice claims.
About the Author
Gregory S. Pokrywka, MD, FACP, FNLA , NCMP, is assistant professor of medicine at Johns Hopkins University School of Medicine and director of the Baltimore Lipid Center, which he formed in 2001. He received his medical degree from Maryland Medical School and was chief resident at Mercy Hospital in Baltimore. He is a boardcertified internist, diplomate of the American Board of Clinical Lipidology, and a fellow of the National Lipid Association. Dr Pokrywka is also a certified menopause practitioner and board member of the South East Lipid Association. Dr. Pokrywka participates enthusiastically in the Go Red for Women and WomenHeart campaigns to fight heart disease in women.
