Publication
Article
Cardiology Review® Online
Statin Usage and All-Cause and Disease-Specific Mortality in a Nationwide Study
Author(s):
Peter H. Jones, MD, FA CP, FN LA
REVIEW
Haukka J, Niskanen L, Partonen T, Lonnqvist J, Tiihonen J. Statin usage and all-cause and disease-specific mortality in a nationwide study. Pharmacoepidemiol Drug Safety 2011. doi:10.1002/pds/2255.
Statins have proved to be a remarkable preventive cardiovas- cular therapy. The Cholesterol Treatment Trialists’ (CTT) Collaborative Group has shown that statin treatment is better than placebo, and that more-intensive treatment is bet- ter than less-intensive treatment for all cardiovascular outcomes (fatal and nonfatal myocardial infarction, coro- nary revascularization, and stroke).1 For every 1 mmol/L (39 mg/dL) reduction in low-density lipoprotein (LDL) cholesterol, there is a 20% to 25% reduction in major cardiovas- cular events as well as a significant reduction in all-cause mortality.1 It is important to note that the CTT meta- analysis included subjects from randomized clinical trials (RCTs), which is a different situation from the real- world clinical setting in which we all practice.
The real-world setting lacks both the inherent motivation found in RCT patients and the dedicated clinical trial personnel who focus on the techniques of medication compliance, adherence, and follow-up, which together can produce a long-term compliance rate of >80%. Therefore, efforts have been made to analyze whether the use of pharmacy records and medical claims/ national medical databases can deter- mine whether varying levels of adherence to statin treatment result in different levels of outcomes benefit (as hard end points, hospitalizations, health care costs, etc). An example of just such an analysis, in a Finnish population, is presented in the study by Haukka et al.
Study Details
The authors used a Finnish nationwide database for a record-linkage study to evaluate the association of statin use with all-cause and disease-specific mortality. The study population of statin users included all residents of Finland who had filled at least 1 prescription of a statin between 1997 and 2005. A control group was chosen, to match the statin users, from the general Finnish population who had not purchased a statin between 1997 and 2005. Adherence to statin use was determined as the proportion of days covered by statin therapy over the follow-up pe- riod, and 7 adherence thresholds were defined: 20%, 30%, 40%, 50%, 60%, 70%, and 80%. The mean length of follow-up was 4.4 years.
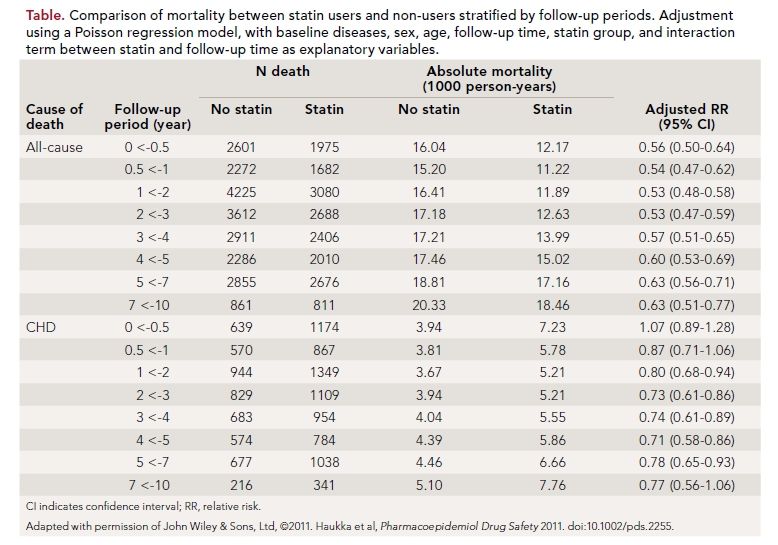
Data for mortality differences between statin users and nonusers by follow-up periods is shown in the table. All-cause mortality was lower in the statin users at the beginning of the follow-up period and persisted over time, but did not fall further. While there was no difference in CHD mortality between the groups at the start of follow-up, a significant benefit became evident for statin users after 1 year. When levels of adherence to statin use was considered, there was no effect on all-cause mortality or non-CHD mortality; however, there was a linear dose-response relationship between increasing statin adherence and decreasing CHD mortality.
The limitations of this study, and others like it, include the possibility of selection bias, as well as the “healthy adherer” effect, such that people who adhere to statin treatment might not only adopt healthier lifestyles but also show greater adherence to other med- ications that can beneficially affect outcomes. This study also had limited ability to assess individual risk factors that contribute to mortality, and, it should be noted, had no information about baseline and follow-up lipid values. This limits the applicability of the results to patients who are clinically determined to be at different levels of baseline CHD risk, and prevents linking the outcomes to the on-treat- ment levels of cholesterol achieved. The authors’ main conclusion was that there was no association between all-cause mortality and statin use, and that non-CHD mortality, especially cancer and suicide, was also not as- sociated with statin use. Most impor- tant, there was a significant reduction in CHD mortality with statin use, and this reduction was linearly proportional to increasing statin adherence.
References
1. Cholesterol Treatment Trialists’ (CTT) Collaboration, et al. Efficacy and safety of more intensive lowering of LDL cholester- ol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670-1681.
2. Marelli C, Gunnarsson C, Ross S, et al. Statins and risk of cancer: a retrospective cohort analysis of 45,857 matched pairs from an electronic medical records data- base of 11 million adult Americans. J Am Coll Cardiol. 2011;58:530-537.
3. Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. J Am Coll Cardiol. 2008;52:1769-1781.
4. Ray KK, Sesbasai SR, Erqou S, et al. Statins and all-cause mortality in high- risk primary prevention: a meta-analysis of 11 randomized controlled trials involv- ing 65,229 participants. Arch Intern Med. 2010;170(12):1024-1031.
5. Ruokoniemi P, Korhonen NM, Helin- Salmivaara A, et al. Statin adherence and the risk of major coronary events in pa- tients with diabetes: a nested case-control study. Br J Clin Pharmacol. 2011;71:766- 776.
6. Pittman DG, Chen W, Bowlin SJ, Foody JM. Adherence to statins, subsequent healthcare costs, and cardiovascular hospi- talizations. Am J Cardiol. 2011;107:1662- 1666. February 2012
Commentary
Evaluating “Real-World” Statin Use
T
his study was performed to evaluate, in a “real- world” cohort of subjects, whether adherence to statin treatment had any beneficial, or even detri- mental, effect on all-cause or disease-specific mortality. The results are certainly not surprising for the benefit on CHD death, but are surprising for the lack of effect on all-cause mortality.
There has never been evidence from previously pub- lished meta-analyses of RCTs that statin treatment has a detrimental effect on non-CHD mortality, especially cancer-specific mortality.2 To the contrary, these meta- analyses suggest reductions in not only CHD mortality but also all-cause mortality in both primary and sec- ondary patient populations.3,4 An important finding ments. Should we focus only on telling them about the health and/or cost benefits of statin use, for instance, and minimize, or even ignore, the potential side effects such as myalgias, Recent data using health claims databases has also shown that adherence to statins reduces cardiovascular hospitalizations and total health care costs.... from this study is that in a population that is not in a con- trolled trial setting, a greater adherence to statin use reduces CHD mortality with- out any trade-off in non-CHD mortality. It could be reason- ably anticipated that if these patients were followed for longer than 4.4 years, the reduction in CHD death observed (without a change in non-CHD death) would result in a reduction in all-cause mortality.
Recent date using health claims databases has also shown that adherence to statins reduces cardiovascular hospitalizations and total health care costs, and that better statin adherence in patients with type 2 diabetes predicts reduced major corinary events. 5,6 Adherence to and persistence with treatments for chronic asympotomatic medical conditions such as hypertension and dyslipimedia are not as optimal as we would like, despite clinically proven benefecial outcomes.
As clinicans, we struggle with finding the best method to encourage our patients to persist with drug tretments. Should we focus only on telling them about the health and/or cost benefits of statin us, for instance, and minimize, or even ignore, the potential side effects such as myalgias, weakness, and hepatic transaminitis, to name a few? What data can we show patients that will convince them that the long-term adher- ence to therapy has overwhelming ben- efit? Real-world da- tabase information, such as this study, can be both reassur- ing and motivating.
For our at-risk patients who can tolerate statins, even with manageable short- term side effects, this study confirms that long-term drug persistence provides one of the single most powerful methods to decrease CHD death, with no trade-off on death from other causes.
About the Author
Peter H. Jones, MD, FACP, FNLA, is medical director of the Weight Management Center at the Methodist Diabetes and Metabolism Institute in Houston, Texas, and associate professor of medicine in the Center for Cardiovascular Disease Prevention at Methodist DeBakey Heart and Vascular Center at The Baylor College of Medicine. Dr Jones received his MD at The Baylor College of Medicine as the Michael E. DeBakey Scholar, where he also completed his internal medicine residency. He is board certified in internal medicine and clinical lipidology and is a fellow of the American College of Physicians and of the National Lipid Association (NLA). He was a board member of the NLA, and served as secretary and president of that organization. He is currently a board member of the American Board of Clinical Lipidology.
