Publication
Article
Family Practice Recertification
Despite Controversy, JNC 8 Guideline Provides Much-needed Standards for Hypertension Management
Author(s):
Many years in the making, but not without controversy, the JNC 8 is a welcomed evidence-based guideline for the management of hypertension.
Frank J. Domino, MD
Review
James PA, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2013 Dec 18. http://jama.jamanetwork.com/article.aspx?articleid=1791497.
Study Methods
This evidence-based guideline was derived from the report of panelists selected from more than 400 nominees. The final Eighth Joint National Committee (JNC 8) panel — which included senior scientists from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and a senior medical officer and senior scientist from the National Heart and Lung and Blood Institute (NHLBI) — consisted of 14 experts in hypertension, 6 in primary care, 2 in geriatrics, 2 in cardiology, 3 in nephrology, 1 in nursing, 2 in pharmacology, 6 in clinical trials, 3 in evidence-based medicine, 1 in epidemiology, 4 in informatics, and an additional 4 in the development and implementation of clinical guidelines.
The panelists based their work on the methods of the non-partisan Institute of Medicine (IOM). During the course of their reports, some members left, presumably in dissent of the panel’s findings.
The JNC 8 panel was charged with answering the following questions in an evidence-based manner:
- In adults with hypertension, does initiating antihypertensive pharmacologic therapy at a specific blood pressure threshold improve health outcomes?
- In adults with hypertension, does treatment with antihypertensive pharmacologic therapy to a specified goal lead to improvements in health outcomes?
- In adults with hypertension, do various antihypertensive drugs or drug classes differ in comparative benefits and harms on specific health outcomes?
Results and Outcomes
This guideline focused on adults aged 18 years and older, so it does not apply to those under 18. Studies were included in the evidence-based review if they reported the effects of interventions on any of the following outcomes:
- Overall mortality, cardiovascular disease (CVD)-related mortality, or chronic kidney disease (CKD)-related mortality.
- Myocardial infarction (MI), heart failure (HF), hospitalization for HF, or stroke.
- Coronary revascularization, including coronary artery bypass graft (CABG) surgery, coronary angioplasty and stent placement, or carotid, renal, or lower extremity revascularization.
- End-stage renal disease (ESRD), the doubling of creatinine levels, and the halving of the Glomerular filtration rate (GFR).
The data included in this study was limited to randomized control trials (RCTs) and based upon content from January 1996 through December 2009, with a follow-up protocol to allow repeat searching from December 2009 to August 2013.
The following recommendations resulted from a systematic review of those high-quality studies:
Recommendation 1: In the general population ≥60 years old, initiate pharmacologic treatment to lower systolic blood pressure (SBP) ≥150 mm Hg or diastolic blood pressure (DBP) ≥90 mm Hg, and treat to a goal SBP of <150 mm Hg and goal DBP of <90 mm Hg [Strong evidence]. If blood pressure-lowering agents are already in place in those ≥60 years old and SBP is <140 mm Hg, then no medications need to be adjusted [Expert opinion]. The JNC 8 panel additionally found treating patients in this age group to a BP goal of <150/90 resulted in reduced stroke, HF, and coronary artery disease (CAD), though lowering SBP <140 mm Hg provided no additional benefit.
Recommendation 2: In the general population <60 years old, initiate pharmacologic treatment to lower DBP ≥90 mm Hg and treat to a DBP goal of <90 mm Hg. The JNC 8 found strong evidence to support this recommendation for those aged 30-59 years old, and felt by expert opinion that it was valid from ages 18 to 29.
Recommendation 3: In the general population <60 years old, initiate pharmacologic treatment to lower SBP ≥140 mm Hg and treat to an SBP goal of <140 mm Hg. Only expert opinion supported this recommendation, as there were no RCTs comparing SBP 140 mm Hg to other levels.
Recommendation 4: In adults aged ≥18 years with CKD, initiate pharmacologic treatment for SBP ≥140 mm Hg or DBP ≥90 mm Hg, and treat to a goal SBP of <140 mm Hg and goal DBP of <90 mm Hg [Expert opinion]. This recommendation also applies to patients <70 years old with an estimated or measured GFR <60 mL/min/1.73 m2; however, the literature did not elaborate on patients >70 years old, so the recommendation does not apply to them.
Recommendation 5: In those aged ≥18 years with diabetes, initiate pharmacologic treatment to lower SBP ≥140 mm Hg or DBP ≥90 mm Hg, and treat to a goal SBP of <140 mm Hg and goal DBP of <90 mm Hg [Expert opinion]. While some data showed improved health outcomes from an SBP goal of <150 mm Hg, no high-quality RCTs met the guideline’s inclusion criteria to support a lower BP level.
Recommendation 6: In the nonblack population, including those with diabetes, initial antihypertensive treatment should include a thiazide-type diuretic, calcium channel blocker (CCB), angiotensin-converting enzyme inhibitor (ACEI), or angiotensin receptor blocker (ARB) [Moderate evidence]. The JNC 8 panel had high standards for RCT inclusion in this recommendation, as it only considered trials comparing one antihypertensive to another. It did not recommend beta-blockers (BB) for the initial treatment of hypertension because one trial focusing on BB use found a higher rate of the primary composite outcome of cardiovascular (CV) death, MI, or stroke compared to the use of an ARB. Alpha-blockers were also not recommended because they were found to worsen cerebrovascular, HF, and combined CV outcomes compared to diuretics.
Recommendation 7: In the black population, including those with diabetes, initial antihypertensive treatment should include a thiazide-type diuretic or CCB [Moderate evidence for blacks without diabetes; weak evidence for blacks with diabetes]. The majority of the support for this recommendation originated from a single large trial that found CCBs were less effective than diuretics in preventing HF in the black population, though there were no differences between CCBs and diuretics in overall mortality or cerebrovascular, chronic heart disease (CHD), combined CV, and kidney outcomes.
Recommendation 8: In the population aged ≥18 years with CKD and hypertension, regardless of race or diabetes status, initial or add-on antihypertensive treatment should include an ACEI or ARB to improve health outcomes [Moderate evidence]. The rationale for this recommendation was based on improved kidney outcomes with an ACEI or ARB, as neither ACEIs nor ARBs improved CV outcomes compared to alpha-blockers or CCBs. The panel relied on expert opinion to support this recommendation in black patients with CKD. As the majority of CKD patients with hypertension will require more than one drug to achieve their goal BP, it is recommended that an ACEI or ARB be used as an initial therapy or second-line therapy added to a diuretic or CCB in black patients with CKD. The JNC 8 also noted that increases in creatinine may occur during ACEI or ARB use, so it recommended monitoring electrolyte and serum creatinine levels after initiating any of those medications and reducing the dose as required.
Recommendation 9: Since the objective of hypertension therapy is to maintain BP control, increasing the dose of the initial drug or adding a second agent is recommended if control is not reached within a month of treatment. However, the JNC 8 panel recommended an ACEI and ARB should not be used together in the same patient. If the BP goal cannot be reached with 2 drugs, then a third medication should be added and titrated. If hypertension cannot be controlled with 3 drugs, then the authors recommended referral to a hypertension specialist, based on its expert opinion.
Commentary
Many years in the making, but not without controversy, the JNC 8 is a welcomed evidence-based guideline for the management of hypertension. This panel — which included not only hypertensive experts, but also those from a variety of specialties — was an outstanding example of mining the best available data and broadest perspective to generate a list of recommendations for a particular condition.
However, the limitations of the recommendations include 2 significant issues, the first of which involves the included data. The JNC 8 panel did not utilize cohort studies, systematic reviews, or meta-analyses in their reviews. While those absences may distort a small sub-segment of the conclusions, the objectivity and insight of the panel allowed for both strong recommendations and honest grading of the outcomes. To include all of the best trial data and address changes in the literature from 2009 through the present, the panelists added a “bridge search” through 2013 to their work, though they found no additional studies that would change their recommendations.
Next, despite the panel’s significant agreement on almost every recommendation, a subset of the authors disagreed with the standard to raise the SBP cutoff from 140 mm Hg to 150 mm Hg in patients aged older than 60 years without diabetes or CKD. A recent summary of this minority group’s rationale1 followed the JNC 8 paper’s release.
But perhaps the greatest JNC 8 controversy is the dissention among the panel members. As the panel’s work was concluding, the NHLBI withdrew from the process and announced it would partner with the American Heart Association (AHA) and the American College of Cardiology (ACC) to review and release new guidelines, which it ultimately decided not to pursue.
While the NHLBI’s rationale has not yet been made public, the presumption for its dissention is the recommendation to increase the cutoff for hypertension diagnosis — from 140 mm Hg to 150 mm Hg — in those over the age of 60. This was unlikely to win the approval of the AHA or ACC, as both groups were considered stakeholders with an inherent bias toward aggressive care, which was at odds with the process the IOM panel agreed to follow. In short, the AHA and ACC were viewed as more apt to rely upon “expert opinion” than to reflect the best data available.
In their defense, the dissenters argued the SBP goal of <140 mm Hg for all patients would keep the US guideline consistent with European and Canadian recommendations, as well as simplify the information providers would need to know. The dissenting panelists also allowed an SBP goal of 150 mm Hg for those aged 80 years or older who are frail, in response to the population’s greater risk for drug-induced adverse events.
The JNC 8 did not request endorsement from the AHA or the ACC, so it did not receive it. The rationale for this approach was the accurately assumed resistance from the AHA and ACC, which subsequently have not supported this guideline. This is unfortunate, as the JNC 7 was published in 2003, and much has changed in patient care over the last 10 years. If all major organizations endorsed one unified set of recommendations, it would leave the medical community on firm ground. Without this consensus, many will wonder how to proceed.
What has not sparked controversy is the recommendation for lifestyle intervention, which suggests all patients must be counseled on a healthy diet, weight control, and regular exercise. However, the JNC 8 did not address the issue of salt, or more specifically, sodium restriction. This has become an area of concern, as current data supporting sodium restriction to control hypertension is based upon short-term observational studies, and long-term data has not been found to support such restriction in hypertension management.2 Avoidance of highly processed and salt-laden foods will continue to be an important dietary recommendation, but unless a patient has CKD or HF, salt restriction will likely play a less important role in overall hypertension management.
Taken together as a whole, the JNC 8 recommendations help all healthcare providers focus on certain priorities regarding hypertension management. Rather than honing in on very low BP levels for hypertension control, solid evidence-based outcomes can now be considered and adopted. This is most important at a time when third-party payers are evaluating quality data and patient outcomes.
The JNC 8 must become the new standard for all quality measures going forward. While some valid arguments have been offered by the guideline’s dissenters, these opinions fall outside of the evidence-based processes utilized by the JNC 8 panel and the IOM. The dissenters’ prognostication of worsening cerebrovascular outcomes is simply conjecture, and only time will tell if these changes can actually occur. Until future data proves otherwise, clinicians should adopt the JNC 8 recommendations, as they were generated from the best clinical evidence available.
References
1. Wright JT, et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014 Jan 14. http://annals.org/article.aspx?articleid=1813288.
2. Mitka M. IOM report: Evidence fails to support guidelines for dietary salt reduction. JAMA. 2013 Jun 26;309(24):2535-6. http://jama.jamanetwork.com/article.aspx?articleid=1700490&resultClick=1.
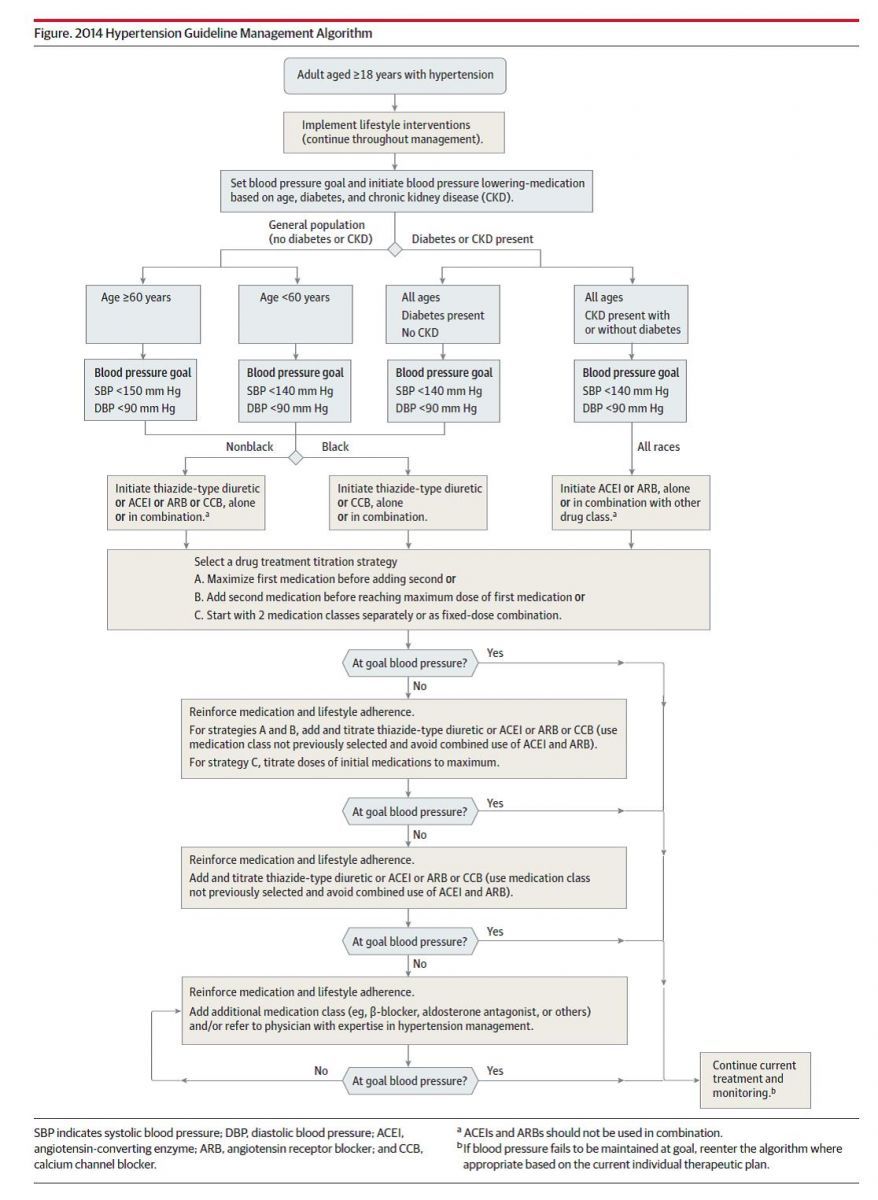
Algorithm
Click the figure to download this handy flowchart of the JNC 8 hypertension management guideline.
Source: James PA, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2013 Dec 18.
About the Author
Frank J. Domino, MD, is Professor and Pre-Doctoral Education Director for the Department of Family Medicine and Community Health at the University of Massachusetts Medical School in Worcester, MA. Domino is Editor-in-Chief of the 5-Minute Clinical Consult series (Lippincott Williams & Wilkins). Additionally, he is Co-Author and Editor of the Epocrates LAB database, and author and editor to the MedPearls smartphone app. He presents nationally for the American Academy of Family Medicine and serves as the Family Physician Representative to the Harvard Medical School’s Continuing Education Committee.